Abbott executive Dr. Nick West believes the company offers the “best-in-class” drug-eluting stent with its Xience platform.
When Abbott (NYSE:ABT) CMO & divisional VP of global medical affairs for its vascular business Dr. Nick West looks back at his use of drug-eluting stents in the early 2000s, all he sees now is innovation.
As a practicing interventional cardiologist, West remembers an earlier time in which the stents were barely deliverable. Each available platform had marked differences and each had its benefits and drawbacks.
“It’s fair to say that, if you look at the world of drug-eluting stents, they’ve evolved enormously,” West told Drug Delivery Business News. “They’ve just changed hugely.”
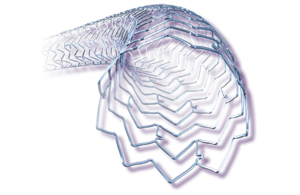
That evolution has led to Abbott’s latest version of its drug-eluting stent platform — the Xience Skypoint — which last month received FDA approval and CE mark and is touted as easier to place while allowing physicians to treat larger blood vessels through improved stent expansion that can open clogged vessels more effectively.
Additionally, Abbott last month received FDA approval for one-month dual antiplatelet therapy (DAPT) labeling using the Xience family of stents, with the FDA’s approval for one-month (as short as 28 days) DAPT labeling applying to high bleeding risk (HBR) patients in the U.S.
The major difference, West says, comes in the form of more than 15 million implants of the stent platform over the years, plus more than 120 clinical trials to back it up.
“The Xience drug-eluting stent platform is probably the class-leading, best-in-class drug-eluting stent,” West said. “It has an unrivaled quantity and quality of data behind it.
“Compared to any other platform — and I’m not just saying this as a promotional thing — we have an unrivaled quantity of data. More than that, we have up to the minute data.”
West said the early days of drug-eluting stents saw dual antiplatelet therapy periods vary from platform to platform, with decisions made less on evidence and more on the original trials conducted.
Six months and four months were early DAPT ranges, while around 15 years ago, concern over higher rates of stent thrombosis was put down to patients not continuing antiplatelet therapy for long enough, so the knee-jerk reaction was to set DAPT time at 12 months with indefinite aspirin treatment after that.
A dichotomy of schools of thought soon came, with one side pushing for longer antiplatelet therapy to reduce the risk of the stent clotting and heart attack, with a downside of a higher risk of a bleeding event. West pointed out that the HBR group of patients, who take a combination of blood thinners for antiplatelet therapy — a large population, given that anyone over the age of 75 is considered a bleeding risk — demonstrate the need for a different avenue with DAPT.
With this in mind, Abbott sought a solution for providing this necessary therapy without keeping the risk of bleeding beyond a month. The company with Xience managed to shorten the duration of dual antiplatelet therapy, first to 90 days and now 28 days, with patients staying on aspirin beyond those time periods.
Studies of both ranges of time showed similar outcomes, with no penalties in ischemic outcome, stents cutting off, heart attacks and the need for revascularization, while the risk of bleeding was lowered.
“We’re not saying everyone should necessarily shorten their antiplatelet therapy,” West said. “We’re saying that, for those patients with HBR, where a bleed can be catastrophic, you can have the security of knowing that you can stop as early as 28 days without penalty.”
Part of the Xience platform’s success, West said, comes from the fact that the platform, rather than undergoing wholesale changes, has remained similar over the years with only slight deviations, meaning the FDA has not required additional investigational device trials for validation.
The platform uses the same fluorinated copolymer with proven antithrombotic qualities, plus everolimus, a cytostatic drug designed to stop cells from reproducing, thus stopping vascular renarrowing or restenosis.
Changes for Xience Skypoint came in the form of better stent retention on the balloon, ensuring that the stent does not come off the balloon during deployment, as West said some stents shorten after deployment. Xience Skypoint was designed not to shorten in any way.
“We’ve now got the whole package,” West said. “We’ve not only got an up-to-the-minute stent platform with all of these great features that make a clinician’s job easier when they’re putting it in, but it’s backed by a vast quantity of clinical data both in terms of safety and efficacy.”
As always, West expects more evolution to come with the Xience platform, although focus may shift from the stent itself — which he said is “about as optimal as it can be” — but to the pharmacology and the use of other technologies, including intracoronary imaging with Abbott’s AI-based optical coherence tomography (OCT) platform for guiding the implant.
West said there’s not necessarily nowhere to go with the stent, but changes can still come down the line.
“We never stand still in terms of innovation,” West said. “We’re always interested in innovating to generate devices that can meaningfully impact patients’ lives. That’s desperately important.”

