 Researchers from Duke University and the Howard Hughes Medical Institute have developed a technique to target and deliver drugs to specific types of neurons in the brain. The team argues that this will enable scientists to more accurately study neurological disease while offering a more targeted treatment method.
Researchers from Duke University and the Howard Hughes Medical Institute have developed a technique to target and deliver drugs to specific types of neurons in the brain. The team argues that this will enable scientists to more accurately study neurological disease while offering a more targeted treatment method.
The current method of treatment for neurological diseases involves dosing all types of neurons, which can blur the study of how cell receptors work and how their manipulation can lead to clinical benefits and side effects.
The team’s method, called DART – Drugs Acutely Restricted by Tethering – could overcome the systematic dosing of standard drugs, the researchers said.
In its 1st study, which was published in the journal Science, the team used DART to study how the AMPA receptor in a mouse model of Parkinson’s disease controls movement difficulties. The researchers said their results showed why a recent clinical trial of an AMPAR-blocking drug failed – and how to improve future work.
“This study marks a major milestone in behavioral neuropharmacology,” principal investigator Michael Tadross said in prepared remarks. “The insights we gained in studying Parkinson’s mice were unexpected and could not have been obtained with any previous method.”
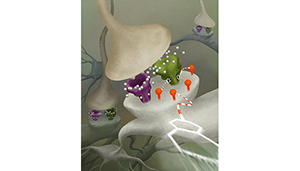
DART genetically programs a specific cell type to express a “GPS beacon” – an enzyme borrowed from bacteria and put on a cell’s surface. Then, the team delivered drugs loaded with what they refer to as a special homing device.
The researchers administered the drugs at very low doses, so they don’t affect other cells. But the drug’s homing system helped the tagged cells’ surface capture the drug. The drug accumulated quickly, at concentrations that are 100 to 1000 times higher than previously observed, according to the team.
In the mouse model of Parkinson’s, the team attached a homing signal beacon to 2 types of neurons – D1 neurons, the “go” command for motor control, and D2 neurons, the “stop” command.
Using the DART method, Tadross and his team delivered an AMPAR-blocking drug to only D1 neurons, only D2 neurons or both.
When the drug was delivered to both cell types, the drugs improved only 1 of several motor dysfunction symptoms, which mirror the results of recent human clinical trials. The team also observed that delivering the drug to just the D1 neurons, the “go” cells, produced no observable outcome.
However, when they targeted the same drug to D2 neurons, the “stop” cell type, the mice’s movements became faster, more frequent and more fluid.
“Already in our first use of DART, we’ve learned something new about the synaptic basis of circuit dysfunction in Parkinson’s disease,” Tadross said. “We’ve discovered that targeting a specific receptor on specific types of neurons can lead to surprisingly potent improvements.”
Next, the team is looking to deliver drugs to neurons using an emerging viral technique. Tadross is also hoping to develop a version of DART that does not use the genetically-added homing beacon.
“All too often in basic science, approaches are developed that may ‘1 day’ make a difference to human health,” he said. “At Duke, there’s a palpable emphasis on providing new treatments to people as quickly as possible. I’m very excited that in this environment, my lab can work collaboratively with scientists, physicians, and biotech to solve the real-world challenges involved.”

