Researchers from the Wyss Institute for Biologically Inspired Engineering at Harvard University have bioprinted a functional 3D renal architecture with living human epithelial cells.
Previously, the team bioprinted tissue constructs made of living cells alongside a vascular network in an extracellular matrix. These constructs are functional in vitro for more than a month.
“The current work further expands our bioprinting platform to create functional human tissue architectures with both technological and clinical relevance,” lead researcher Jennifer Lewis said in prepared remarks.
The 3D renal architecture mimics a vital component of the nephron – the proximal tubule. A human kidney has over 1 million nephrons that are responsible for transporting nutrients from renal filtrate back into the bloodstream.
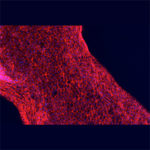
In a study published today in Scientific Reports, researchers describe the technique they used to construct the functioning renal architecture. Using “fugitive ink,” they bioprinted a tubular shape similar to the structure of natural renal proximal tubules. The ink was encapsulated by layers of an extracellular matrix and was removed after the construct cooled. Researchers perfused the system’s inlet and outlet with cell growth medium and human proximal tubule cells.
They found that the nutrients could nourish the cells and sustain them for more than 2 months. As the cells matured, the researchers reported that the 3D architecture began to perform the same duties as a natural proximal tubule. The construct could be used as a patient-specific tool for clinicians to assess a treatment plan or for pharmaceutical companies to evaluate a compound’s effect on a human kidney.
“We have initially targeted this renal architecture, because the kidney represents such a pressing clinical need across the world,” Lewis said. “While thus far we have merely demonstrated a functioning subunit within the kidney, we are actively scaling up the method and its complexity to enable future in vivo applications.”
“This advance in 3D printing of living tissues that recapitulate crucial organ functions by Jennifer and her team opens a new path to engineering model systems for drug development, as well as for creating more functional extracorporeal devices and whole organ implants in the future,” founding director Dr. Donald Ingber said.
