 Researchers from Northwestern University have developed a 3D-printed vascular stent that can be personalized to the patient, the school reported this week.
Researchers from Northwestern University have developed a 3D-printed vascular stent that can be personalized to the patient, the school reported this week.
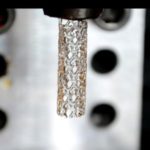
The stents are made of a biodegradable, citric acid-based polymer that researchers could load with drugs to release slowly as the blood vessel wall heals.
“Right now, the vast majority of stents are made from a metal and have off-the-shelf availability in various sizes,” lead researcher Guillermo Ameer said in prepared remarks. “The physician has to guess which stent size is a good fit to keep the blood vessel open. But we’re all different and results are highly dependent on physician experience, so that’s not an optimal solution.”
The 3D-printing technique that Ameer used is called projection micro-stereo-lithography. Researchers shine a pattern of light onto the polymer, converting it to a solid that slowly displaces to cure the next layer of polymer. The high-resolution technique can print features as small as 7 microns and can print 100 stents at a time, according to the study that the team published in Advanced Materials Technologies.
“There are cases where a physician tries to stent a patient, and the fit is not good,” he explained. “There might be geometric constraints in the patient’s vessel, such as a significant curvature that can disturb blood flow, causing traditional stents to fail. This is especially a problem for patients who have conditions that prevent the use of blood thinners, which are commonly given to patients who have stents. By printing a stent that has the exact geometric and biologic requirements of the patient’s blood vessel, we expect to minimize the probability of these complications.”
In the future, the university reported, the team hopes to investigate how long it takes for the stent to break down and absorb into the body, as well as pursue designs that improve the stent’s long-term performance.
“Not only can we customize the stent for a patient’s blood vessels,” he said, “but we can create all new types of patient-specific medical devices that could make the outcomes of surgical procedures better than what they are today.”

